Navigating Night-Time Wetting: A Guide for Parents and Carers
7/23/20255 min read
Nighttime Bedwetting (Nocturnal Enuresis)
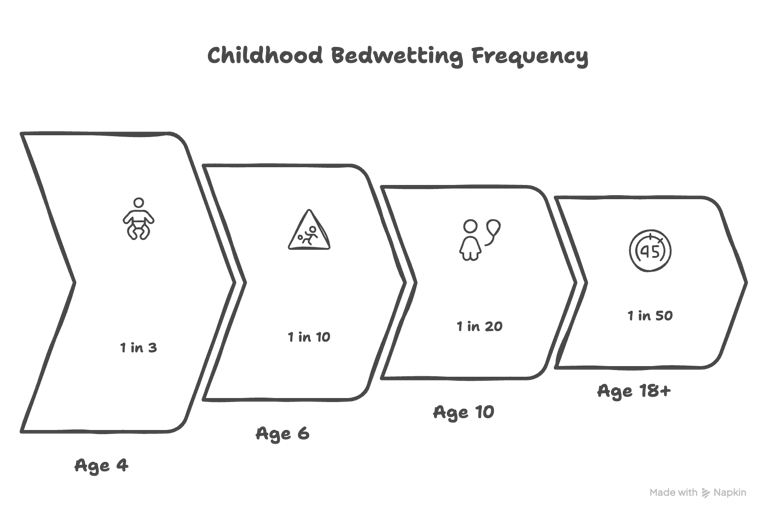
If you’re a parent of a child who wets the bed, it’s important to know you are not alone. Bedwetting, also known as nocturnal enuresis, is an incredibly common part of childhood. It’s not a “problem” that needs fixing, but rather a developmental stage. Consider its natural trajectory:
about 1 in 3 four-year-olds,
1 in 10 six-year-olds, and
1 in 20 ten-year-olds wet the bed.
It can even persist for about 1 in 50 adults.
The most important thing to remember is that it is not your child's fault. Children do not wet the bed on purpose, and a calm, reassuring approach is always best. This guide is designed to provide you with a clear, evidence-based approach to understanding and managing bedwetting, empowering you and your child on the journey to dry nights.
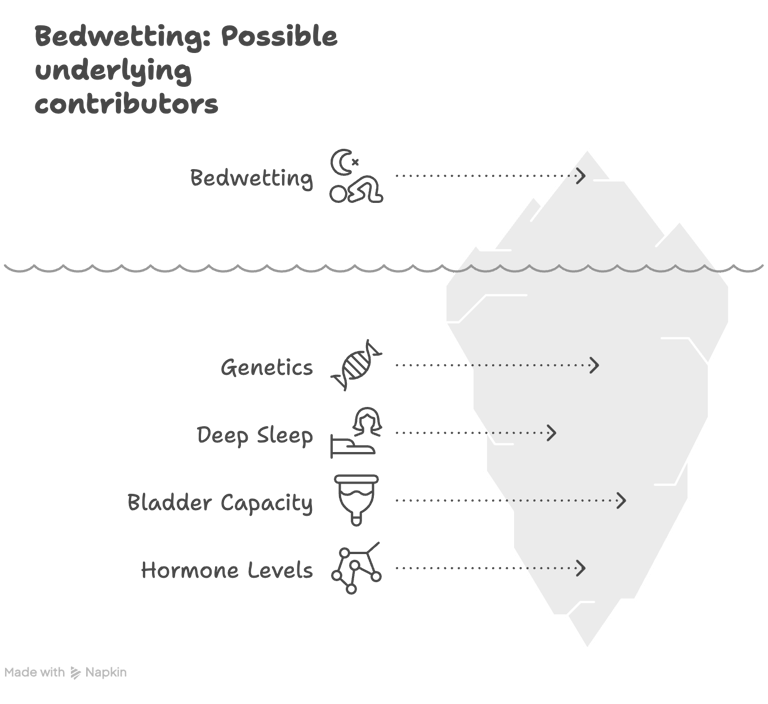
Why Does Bedwetting Happen?
Night-time bladder control is a developmental step that takes longer to achieve than daytime control. It's often a combination of factors:
Genetics: Bedwetting often runs in families. If a parent wet the bed, their child is more likely to.
Deep Sleep: Some children are very deep sleepers and don't wake up to the signal of a full bladder.
Bladder Capacity: A child’s bladder might not yet be large enough to hold all the urine produced during the night.
Hormone Levels: Some children produce less of the night-time hormone (antidiuretic hormone or ADH) that tells the kidneys to make less urine while they sleep.
Primary vs. Secondary Bedwetting: When to Investigate Further
It's helpful to understand what kind of bedwetting your child is experiencing.
Primary Enuresis: This is the most common type, where a child has never been consistently dry at night for a period of six months or more. This is typically developmental.
Secondary Enuresis: This is when a child starts wetting the bed again after having been dry at night for at least six months.
If bedwetting is a new concern (secondary), it’s important to explore possible underlying causes with your GP. Some examples of these could include:
Diabetes: Symptoms could include unusually excessive thirst or urination during the day.
Constipation: Symptoms could include passing hard pellets/pebble like bowel motions, blood in stool, having to strain. Note that a full bowel can press on the bladder and is a very common cause of loss of urine control.
Obstructive Sleep Apnoea (OSA): Symptoms could include loud snoring, pausing in breathing, or gasping at night?
New Psychological Stressors: These could be numerous. Examples include: having a new sibling, starting school, or family changes.
Your GP can help differentiate between common primary bedwetting and other causes that may need attention.
The First Steps: Getting the Basics Right
Before starting any specific treatment, it’s essential to set the stage for success. Understanding your own perception as a parent is key; reassurance and de-stigmatizing the issue for your child is the first and most important step.
Manage Fluid Intake: Ensure your child drinks plenty of fluids throughout the day. Restricting fluids can actually make things worse. Aim for regular drinks, with the bulk of fluids consumed earlier in the day. Cut out caffeine-based drinks.
Good Toileting Habits: Encourage your child to use the toilet 4 to 7 times throughout the day and always right before sleep.
Check for Constipation: If you suspect constipation, managing this should be the first priority.
The Gold Standard: Bedwetting Alarms
For a motivated child and family, a bedwetting alarm is the most effective treatment for achieving long-term dryness. Its success, however, depends entirely on whether the child and family are ready for the commitment.
How Do They Work?
The biological mechanism isn't perfectly understood, but alarms work by conditioning the brain. A moisture sensor in the underwear triggers an alarm at the first drop of urine, training the child to associate a full bladder with waking up.
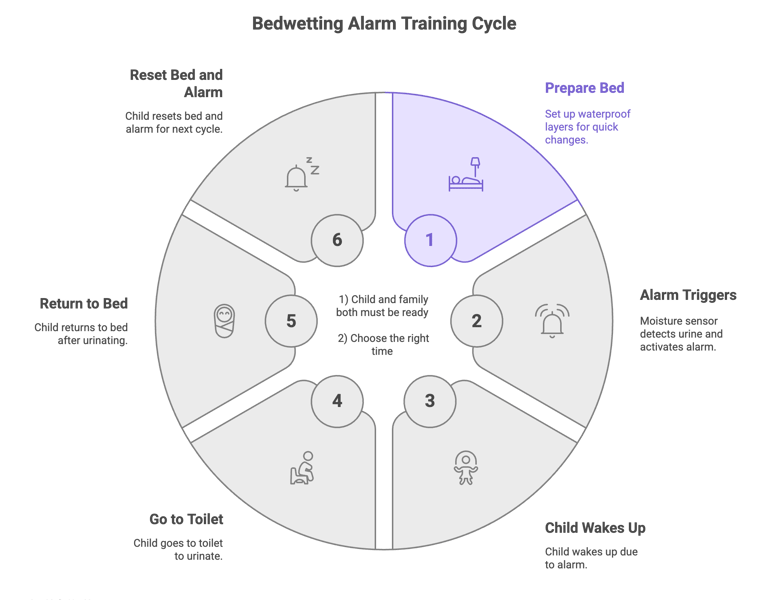
How to Use an Alarm Successfully:
Prepare the Bed: Use a few layers of waterproofing so changes are quick. A common method is waterproof sheet --> regular sheet --> waterproof sheet -->regular sheet.
The Night-time Routine: When the alarm goes off, the child must get up, walk to the toilet to finish urinating, then return to bed. The wet top sheet and protector are peeled off, the alarm is reset on clean underwear, and they go back to sleep.
Note:
Be Patient: The first two weeks are often hit-and-miss. It’s important to commit to trying for at least four weeks. There is a moderate relapse rate, but you can always restart the alarm if needed.
Timing is Everything: Don't start alarm training during a busy or stressful time period, like over Christmas or during exams.
When Alarms Aren't Suitable: Medications
If an alarm isn't suitable, or if a short-term solution is needed for an event like a school camp, medication is an option.
Desmopressin (also known as DDAVP):
This is not a cure, but a "band-aid" that manages the symptom.
It works by mimicking the natural hormone that reduces night-time urine production.
Use & Dosing:
It is often used as a short-term solution.
In Australia, it maybe subsidised for children who have failed alarm treatment or those who have a neurological issue that prevents alarm use.
The starting dose is typically a 120 microgram sublingual wafer (melts under the tongue), which can be increased to 240 micrograms.
Note: It should be taken about one hour before bed.
CRITICAL SAFETY INFORMATION:
Desmopressin is a fairly safe medication.
Desmopressin works for about eight hours, during which the child's body cannot regulate its salt-water balance properly. It is essential to restrict all fluids from one hour before taking the tablet until at least eight hours afterwards to prevent dangerously low sodium levels.
More DOES NOT mean more dry!
When Should You See a Doctor?
While bedwetting is usually a developmental issue, you should see your GP for assessment if:
Your child is over seven and the bedwetting is bothering them.
Your child has daytime symptoms as well as night-time wetting.
Bedwetting starts suddenly after being dry for over six months (secondary enuresis).
You notice any of the potential secondary causes mentioned above.
You are concerned and need reassurance or guidance.
References
Behavioural interventions including alarms: bedwetting (enuresis). (2014). The Royal Australian College of General Practitioners.
Bedwetting in under 19s. (2010). National Institute for Health and Care Excellence (NICE).
The Royal Children's Hospital Melbourne. (n.d.). Bedwetting. Kids Health Info.
The Royal Children's Hospital Melbourne. (n.d.). Enuresis - Bed wetting and Monosymptomatic Enuresis. Clinical Practice Guidelines.
Perth Children's Hospital. (n.d.). Prereferral guidelines: Enuresis.
The Sama GP
Achieving Health Balance,
Together
COMMUNITY
Disclaimer
© 2025. All rights reserved.
NAVIGATE
The information on this website is for educational purposes only and is not a substitute for professional medical advice. Always consult with a qualified healthcare provider for any health concerns.
